Examining the Execution Gap between Knowledge and Lifestyle Change in U.S Chronic Diseases.
- Celine D

- Sep 13, 2025
- 2 min read
Updated: Sep 15, 2025

What Problem are we trying to solve?
According to the CDC, out of the 4.9 trillion dollars spent on healthcare annually, chronic diseases like heart diseases, cancer and diabetes account for a majority of that cost. About 60% of the American population has at least one chronic disease - that’s 201 million with a diagnosed chronic disease out of the 336 million Americans.
Many of these chronic diseases are preventable with a few but pertinent lifestyle changes like good nutrition, physical activity, changes in smoking and alcohol use. So, if health education campaigns, doctor’s office pamphlets, and national awareness programs have been running for decades, why are preventable chronic diseases still climbing?
This project explores the execution gap: the disconnect between knowing what to do and actually being able to do it.
Objectives
Does health education (knowledge) lead to better lifestyle behaviors?
Do emotional, social, and environmental barriers like poor mental health access, high costs, or lack of support systems block people from acting on what they know?
Do these barriers weaken the effect of education, making knowledge less useful in practice?
How do behaviors and barriers together explain the chronic disease burden across U.S. states?
Hypotheses
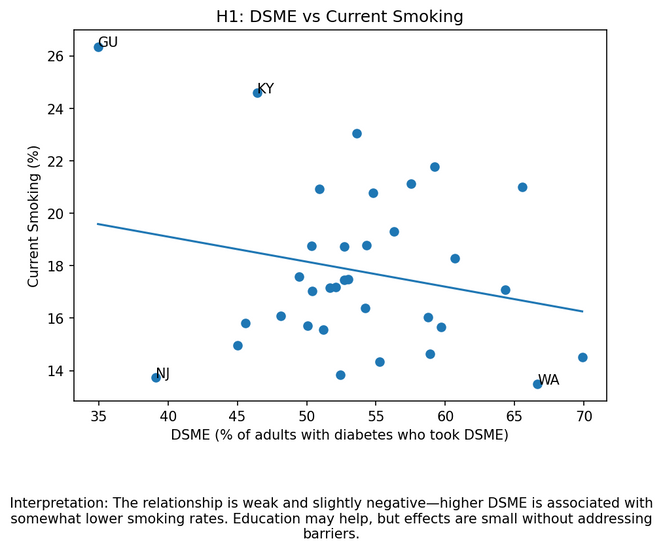
H1. Knowledge Helps: People who receive disease-specific education (e.g., diabetes self-management classes) show modestly healthier behaviors.
H2. Barriers Hinder: Barriers (poor access, stress, poverty, food environment) are strongly linked to unhealthy behaviors.
H3. Moderation: The positive effect of knowledge is weaker when barriers are high and stronger when barriers are low.
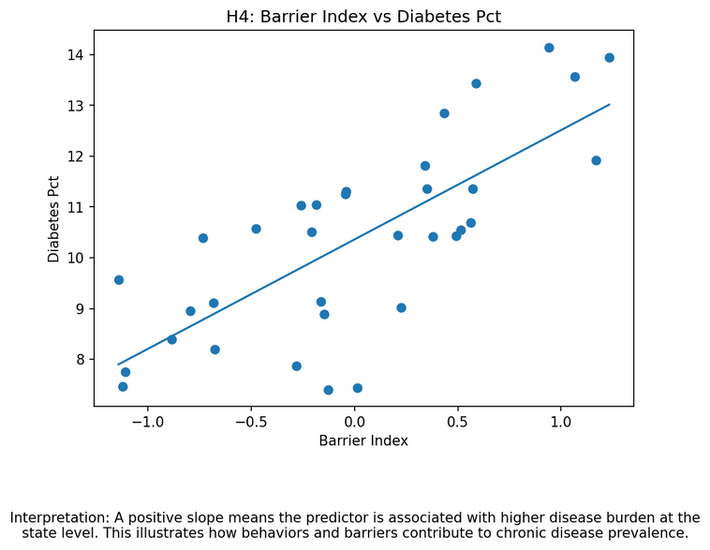
H4. Outcomes: Behaviors and barriers together explain much of the chronic disease burden.
Conceptual Framework

Methods
I analyzed the CDC’s BRFSS 2017 survey data (over 450,000 respondents), combining:
Knowledge: Diabetes Self-Management Education (DSME) participation.
Barriers: Mental health distress, insurance coverage, personal doctor access, and cost barriers.
Behaviors: Physical inactivity, obesity, smoking.
Outcomes: Diabetes and hypertension prevalence.
Using regression analysis and interaction models, I tested whether barriers weaken the link between knowledge and healthy behaviors.
Key Findings
Knowledge helps a little, but only modestly.
States with higher DSME (diabetic self-management education) participation had slightly lower physical inactivity, but effects on obesity and smoking were weak.
Barriers Strongly hinder healthy behaviors.
Poor access and distress strongly predicted worse behaviors (e.g., more inactivity, more smoking).
Knowledge × Barriers reveals the execution gap.
The benefit of knowledge shrinks when barriers are high confirming the execution gap.
Behaviors + barriers together explain much of chronic disease burden.
Diabetes and hypertension rates were best explained by behaviors + barriers, not knowledge alone. These scatterplots show how behaviors (no activity, obesity, smoking) and barriers together explain disease outcomes (diabetes, hypertension).
Contribution
This study shows that education is necessary but not sufficient. Without tackling barriers like mental health support, affordability, and access—knowledge alone won’t close the chronic disease gap.
Policy implication: Funding should shift from awareness-only campaigns to execution-support programs that help people act on the knowledge they already have.
Project Code and Appendix




























Comments